75% of the health infrastructure in India – including doctors and specialists and other health resources – is concentrated in urban areas that contains only 27% of its residents.
An estimated 70% (0.8 billion) of India's 1.2 billion, however, live in Rural India and yet, there is a chronic lack of proper medical facilities for them.
The World Health Organization recommends an estimated 1:1000 doctor-population ratio. In rural India this ratio is under 0.3:1000.
Gross shortage in Health Workforce is the reality of Rural India.
The poor public health infrastructure discourages many Indians from seeking healthcare until a medical emergency demands it, and this in turn allows easily treatable conditions to morph into life-threatening and financially draining, events.
With the ubiquitous use of mobile phones and increased vehicular access in rural India, there is now an opportunity to minimize the divide and contribute to the advancement of healthcare services across rural societies. Additionally, thanks to advancing Machine Learning and Geospatial technologies, it is now possible to combine important social, behavioral and environmental data to predict infection and disease prevalence patterns and accordingly customize ways to provide health information and healthcare. This potent combination of factors significantly improves health outcomes across entire populations.
Our team brings together the perfect ingredients to illustrate and realize the above scenario.
Dr. Thaikkendiyil is a board certified pediatrician and has 'boots on the ground' experience in working with rural populations in Tamil Nadu. She realizes the fact that creating an app, as cool as that may be, will on its own, not be able penetrate a market hampered by lack of high-speed connectivity and different user interaction models. Making a platform for anything built in isolation, far from the problem is a recipe for failure. With her direct experience providing last mile primary care in rural Tamil Nadu she has shaped the technology to fit with the flow of rural life, while adhering to evidence-based care protocols.
Krishna Kumar has a Master's Degree in Medical Informatics and leverages his 17+ years' experience in Software Development to build a scalable Geospatial machine learning and population health surveillance platform that is simply and seamlessly accessed by established, on-ground technologies like SMS and telephony to help deliver rapid and vital real-time information and connect communities to lifesaving services.
Our implementation of the mHealth vision is along 4 quadrants:
Preventive care
Episode self-reporting
Continuity of care
Reactive care
PREVENTIVE CARE:
Public education is the most critical element of any overall strategy for disease control.
Our Machine Learning model combines historic occurrence events, environmental factors, epidemiological trends and episodic self-reported data to assign a risk factor to a community, family or individual.
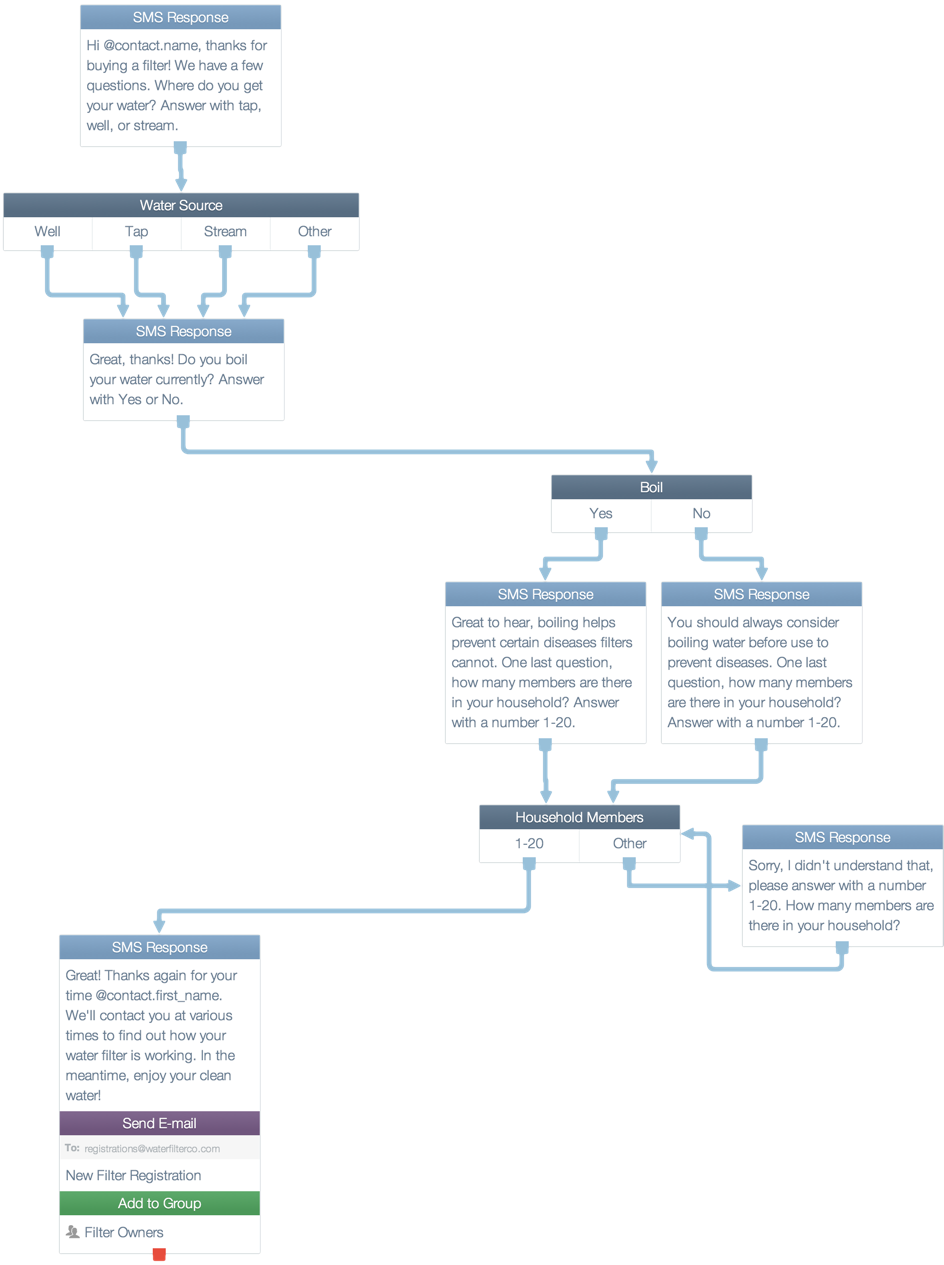
If the risk factor is greater than the disease threshold, an SMS or an automated phone call (depending on whether or not they are literate) is placed to the person/family telling them to take the necessary precautions and asking them if they have the required supplies to do so.

For eg., a common problem in Southern India in the prevalence of Dengue Fever. If a community is flagged as a high-risk, then, the residents are alerted about the condition and are urged to take measures like empty stagnant water and prevent mosquito bites. They are then polled to see if they have adequate protection from mosquitoes like mosquito nets.
If they respond that they don't, a list of those needing the supplies across communities is consolidated and relief measures can be taken to ensure that communities have the necessary items that they need. Information on collecting such items when they arrive are also communicated to the individual residents/families.
EPISODE SELF-REPORTING:
Dedicated primary care can stave off many medical emergencies, however it must be caught early before it morphs into something more serious.
The preventive alerting system is sufficient in and of itself to keep a lot of diseases at bay - however, inevitably, illness does strike. Our self-reporting mechanism makes it easy to report the issue using SMS or a phone call. This will alert the local primary health center and the patient will be told to report to the dispensary for follow-up. This episode also gets tracked and overall population aggregates are gleaned to track the emergence or spread of disease in real-time. In extreme cases, in cases of epidemics, it can act as an early warning system before traditional reporting mechanisms kick in. Additionally, the self-reported data can help determine the rate of spread of the disease and help inform quarantine arrangements and signal the need for medical reinforcements.
CONTINUITY OF CARE REGIMEN / CHRONIC DISEASE MANAGEMENT:
A treatment plan is only as effective as how strictly the patient follows it.
In order to ensure that the evidence-based care regimen (as entered by their doctor in the local dispensary) is being followed consistently, the system reminds them to take the medication at the prescribed times. Multiple studies in this field have proven that a simple reminder system as the one above shows significant effects on patients' adherence.
REACTIVE CARE / ACUTE CARE DIAGNOSIS:
In some cases, there is no option but to get a consult from a physician or a specialist and it is in these scenarios that the divide between urban and rural settings are greatly amplified.
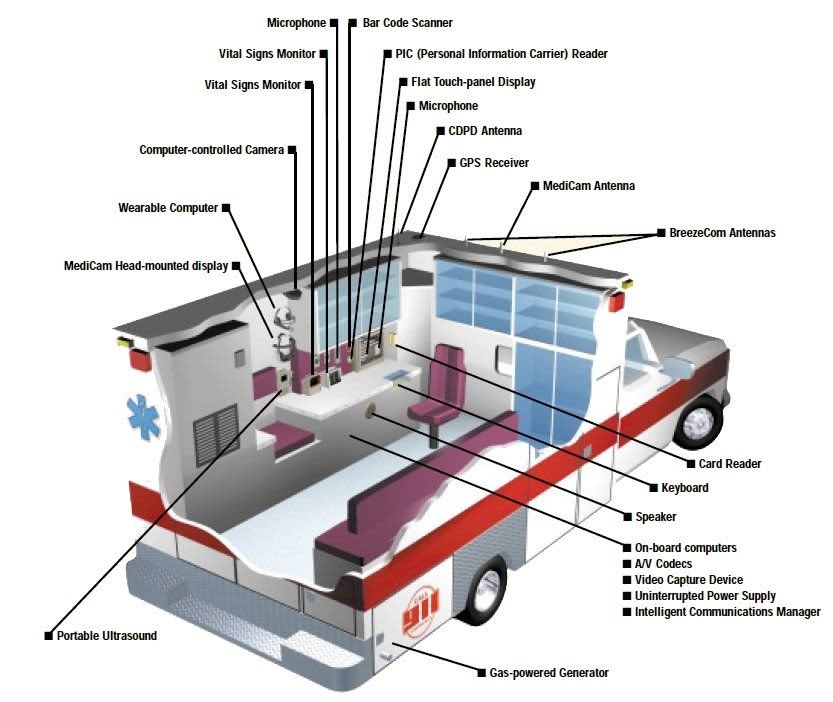
For those that need to be 'seen' by a specialist or a physician with experience beyond the local practitioner, we recommend a mobile tele-medicine system – ideally, a ford vehicle outfitted with an intelligent uplink and a telemedicine system that offers not only direct live transmission of voice and video ( "A picture is worth a thousand words, but perhaps a video is worth a million words." ) but complete patient physiologic data, e.g. ECG, 12-lead STEMI, blood gases, ultrasound, e-PCR, EHR, blood pressure etc. This would be the perfect substitute to the drudgery of going to the nearest hospital and waiting for their attendings and referrals to specialists. Here, based on an initial triage, the specialist can be brought in virtually to directly to address the issue.
Finally, for the minority of cases requiring 'hands-on' operations, they can either be driven out to the town health centers (similar to the Ford SUMURR project) or alternately, there can be an organized deployment of a Mobile Primary Care Unit (MPCU) for delivering primary care via EMS providers. Community Paramedicine may not only reduce healthcare delivery costs, but it also increases the quality of individual patient care.
OPERATIONS:
All of the above scenarios are monitored using a web based dashboard and actions can be initiated from there based on observed data and Machine Learning based predictions, including using OpenXC to grade the terrain to the destination and matching an appropriate driver to the level of driving difficulty. Additionally, OpenXC is used to track the medical service vehicles' whereabouts and accordingly, helps schedule them out to the various communities.




Log in or sign up for Devpost to join the conversation.